When we think about how the brain communicates with the rest of the body, the gut is often overlooked. Yet the gut–brain connection is one of the most active communication systems we have. That “gut feeling” you get during stress, excitement, or worry isn’t your imagination—it’s your nervous system and digestive system talking to one another.
Those familiar butterflies, stomach knots, or sudden appetite changes during stressful moments are powerful examples of how closely the gut and brain interact. This connection not only influences digestion but also plays a significant role in shaping mood, emotional balance, and overall mental well-being.

Environmental factors like diet, stress, and lifestyle directly affect the gut–brain axis (GBA)—a two-way communication system linking the digestive tract to the central nervous system through neural, hormonal, and immune pathways (Mayer et al., 2022). This ongoing exchange helps regulate digestion, immunity, mood, and even sleep.
At the centre of this network is the gut microbiota, trillions of microbes that support digestion while also sending chemical and electrical signals to the brain. This signalling process, known as interoception, helps the brain sense and respond to what’s happening inside the body (Mayer et al., 2022). These microbial messages influence motivation, emotions, and how we cope with stress.

Deep within the digestive tract lies the Enteric Nervous System (ENS)—often called our second brain—containing over 100 million nerve cells (Johns Hopkins, 2025). When we’re relaxed, the ENS keeps digestion running smoothly. But during stress, the brain can override gut reflexes, creating sensations like tightness, nausea, or “gut feelings.
Together, the microbiome, ENS, and brain form a dynamic system where the health of one affects the others, shaping not only physical digestion but also emotional and psychological health.
Research continues to show how powerfully the microbiome shapes mental health:
A study by Taylor et al. (2020) found that higher fruit intake—especially nutrient-rich, fiber-dense fruits—was associated with lower depression scores, particularly in men.
Dietary fiber supports the growth of Bifidobacterium, a beneficial “psychobiotic” linked to improved mood. Conversely, a low-fiber diet favors the growth of Enterobacteriaceae, a bacterial group associated with increased depressive symptoms.

A review by Huang and colleagues (2019) highlighted that both Major Depressive Disorder (MDD) and Bipolar Disorder (BD) are associated with altered gut microbial diversity. Individuals with major depressive disorder, in particular, showed a decrease in microbial richness—suggesting that a disrupted gut environment may contribute to emotional dysregulation.

Up to 95% of serotonin, known for regulating mood and emotional well-being, is produced in the gut (Kim & Camilleri, 2000). Gut bacteria also influence dopamine, another key neurotransmitter linked to motivation and pleasure. Certain bacteria—such as Bifidobacterium—play supportive roles in dopamine production (Hamamah et al., 2022).
In short, when the gut is balanced, it supports clearer thinking, steadier mood, and more resilient stress responses. When disrupted, emotional symptoms can intensify.
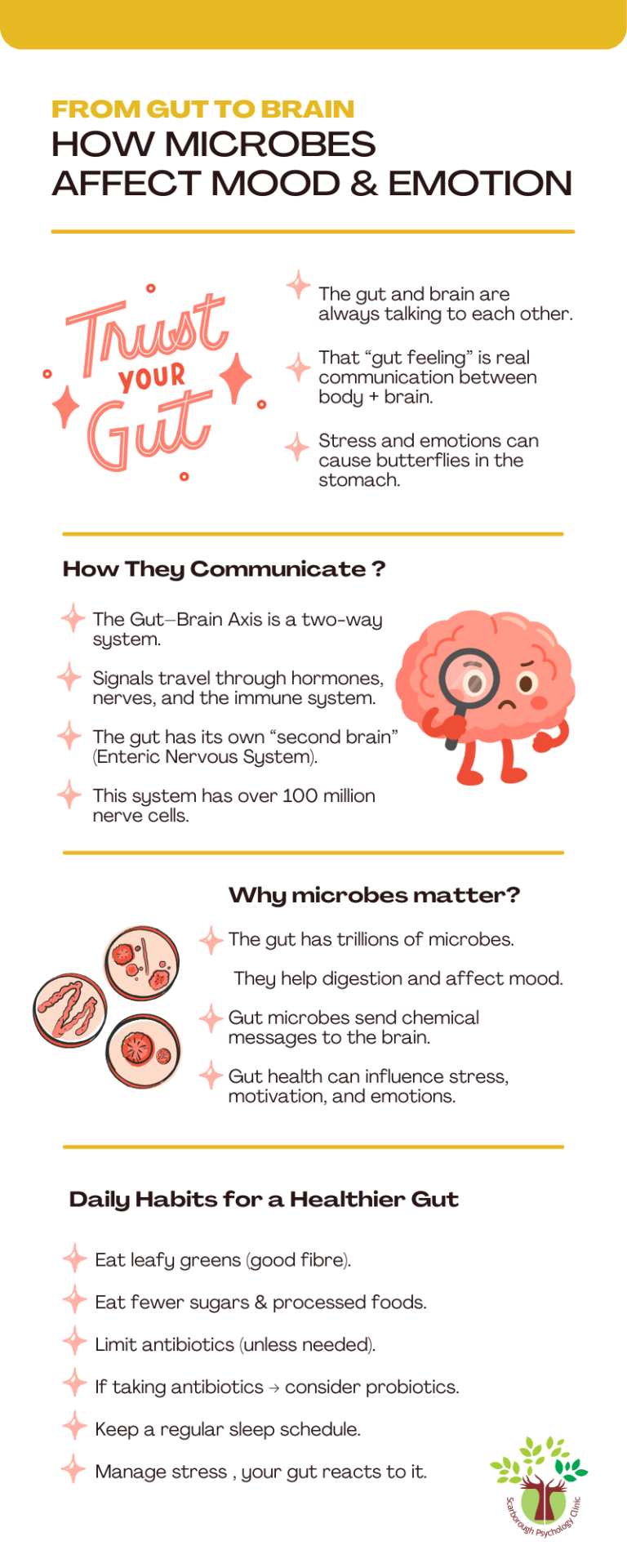
If the gut plays such a crucial role in mental health, how can we nurture it compassionately and sustainably? The Canadian Digestive Health Foundation recommends several practices to strengthen the microbiome:
✔ Eat more leafy green vegetables. Rich in fibre, they help beneficial microbes thrive.

✔ Reduce sugar and processed foods. Simple sugars are absorbed too quickly, leaving little nourishment for gut bacteria.
✔ Use antibiotics mindfully. While antibiotics fight infections, they also wipe out good bacteria. Pairing them with probiotics can help restore balance.

✔ Prioritize regular sleep. Irregular sleep disrupts microbial rhythms and may increase inflammation
✔ Build daily stress-reduction habits. A calmer mind supports a healthier gut—and a healthier gut supports emotional resilience. If stress feels overwhelming, professional support can help restore balance.
Caring for your gut means caring for your mood, your emotions, and your overall well-being. The gut–brain connection reminds us that mental health is deeply intertwined with the body, and small daily habits can create meaningful change over time. If you’re struggling with mood, anxiety, or chronic stress, support is available—and healing often begins with understanding how your body and mind work together.
If you’re noticing changes in your mood, stress levels, or overall emotional balance, you don’t have to navigate it alone.
Book a consultation with Scarborough Psychology Clinic —Compassionate Care for a Brighter Tomorrow.
Allan, S. (2024, April 23). 10 ways to strengthen your microbiome. Canadian Digestive Health Foundation. https://cdhf.ca/en/10-ways-to-strengthen-your-microbiome/
Hamamah, S., Aghazarian, A., Nazaryan, A., Hajnal, A., & Covasa, M. (2022). Role of Microbiota-Gut-Brain axis in regulating dopaminergic signaling. Biomedicines, 10(2), 436. https://doi.org/10.3390/biomedicines10020436
Huang, T., Lai, J., Du, Y., Xu, Y., Ruan, L., & Hu, S. (2019). Current understanding of gut microbiota in mood disorders: An update of human studies. Frontiers in Genetics, 10, 98. https://doi.org/10.3389/fgene.2019.00098
Kim, D., & Camilleri, M. (2000). Serotonin: a mediator of the Brain–Gut connection. The American Journal of Gastroenterology, 95(10), 2698–2709. https://doi.org/10.1111/j.1572-0241.2000.03177.x
Mulder, D., Aarts, E., Vasquez, A. A., & Bloemendaal, M. (2023). A systematic review exploring the association between the human gut microbiota and brain connectivity in health and disease. Molecular Psychiatry, 28(12), 5037–5061. https://doi.org/10.1038/s41380-023-02146-4
Taylor, A. M., Thompson, S. V., Edwards, C. G., Musaad, S. M., Khan, N. A., & Holscher, H. D. (2019). Associations among diet, the gastrointestinal microbiota, and negative emotional states in adults. Nutritional Neuroscience, 23(12), 983–992. https://doi.org/10.1080/1028415x.2019.1582578
The Brain-Gut connection. (2025, October 3). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-brain-gut-connection