Why men’s mental health deserves more attention—and how stress quietly affects hormones and men’s mood and overall well-being.
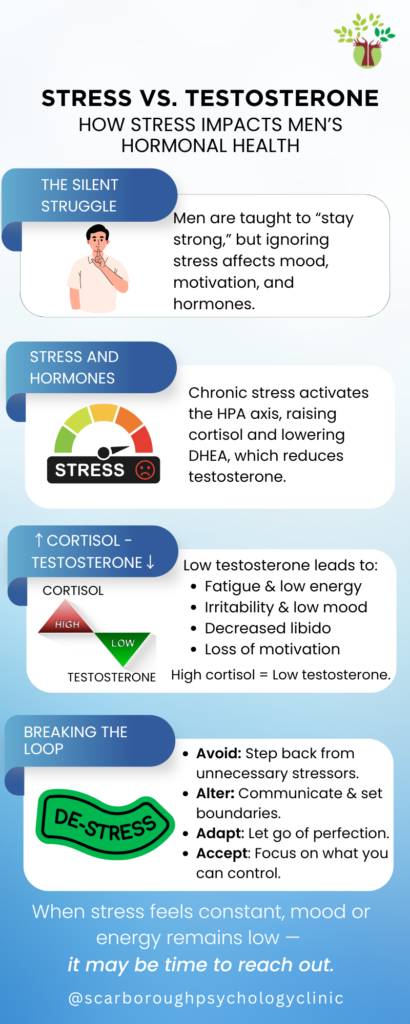
Men are often taught to “handle it,” to push through exhaustion, hide emotions, and stay strong no matter what. But the truth is, stress doesn’t disappear when ignored. It shows up in the body through fatigue, mood swings, low motivation, or even changes in libido.

While short-term stress can sharpen focus, chronic stress tells a different story. Over time, it reshapes how the body functions—influencing hormones and men’s sleep, mood, and long-term health (American Psychological Association).
When stress appears, whether from work pressure, financial strain, or family tension, the brain activates the hypothalamic-pituitary-adrenal (HPA) axis, a feedback loop that releases cortisol, often called the “stress hormone.”
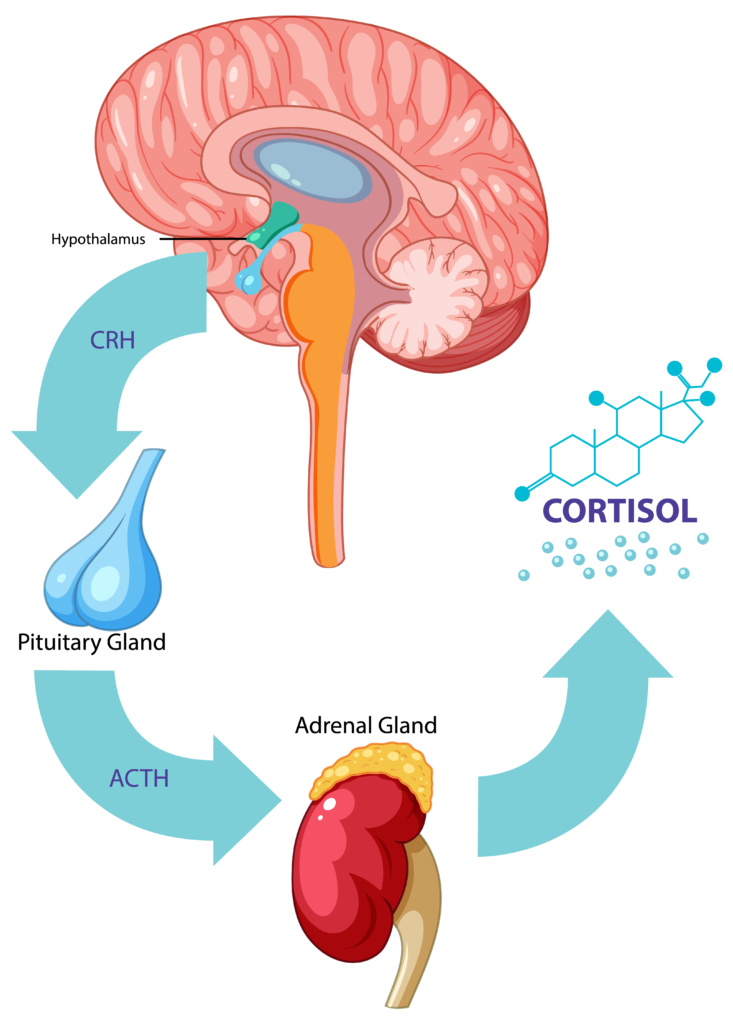
Cortisol’s job is to prepare the body for action, but when levels remain high, it starts to interfere with the endocrine system—a network of glands that regulates hormones in men across the body.
The adrenal glands, located above the kidneys, release both cortisol and dehydroepiandrosterone (DHEA), a precursor to testosterone in men and estrogen in women. Chronic stress increases cortisol but decreases DHEA, creating a hormonal imbalance that directly affects testosterone production.
Cortisol and testosterone operate like a seesaw: when one rises, the other often falls. Scientific studies have confirmed that sustained stress reduces testosterone by suppressing the hypothalamic-pituitary-gonadal (HPG) axis, which manages reproductive hormones (Zueger et al., 2023; Acevedo-Rodriguez et al., 2018).
Normally, the hypothalamus releases gonadotropin-releasing hormone (GnRH), prompting the pituitary gland to secrete luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones stimulate the testes to produce testosterone and sperm.

Testosterone plays far more roles than most people realize. It supports muscle mass, bone density, metabolism, motivation, and emotional balance (Rojas-Zambrano et al., 2025; Cleveland Clinic, 2022).

When testosterone levels fall, men may experience:
Research from JAMA Psychiatry found that testosterone therapy reduced depressive symptoms in men, suggesting a clear link between testosterone and mood regulation (Walther et al., 2018).
Animal studies further show that testosterone enhances serotonin activity, the “feel-good” neurotransmitter, which helps buffer depressive effects.
Similarly, Zitzmann (2020) found that low testosterone levels are associated with higher anxiety, restlessness, and emotional instability, whereas healthy levels can support stress resilience and reward processing.

“Many men don’t realize that chronic stress isn’t just emotional; it’s hormonal. When your body stays in survival mode too long, your mind and hormones both start to pay the price.”
— Dr. Arpita Biswas, Clinical Psychologist
When stress lowers testosterone, it doesn’t just affect the body—it also impacts motivation, patience, and emotional well-being. This can lead to burnout, relationship strain, and self-doubt, which in turn increase stress further.
This stress-hormone feedback loop can become self-reinforcing: cortisol stays high, testosterone stays low, and both mental and physical health begin to suffer. Breaking this loop means caring for both mind and body, through stress reduction, emotional awareness, and professional support when needed.

— Another place hormones and men naturally intersect.
The Mayo Clinic Health System suggests a simple but effective approach called the 4 A’s of Stress Relief (Conway, 2021):
Avoid: Identify and reduce unnecessary stressors. Step away from toxic dynamics or overcommitments when possible.
2. Alter: Communicate clearly and assertively. Setting healthy boundaries helps reduce emotional overload.
3. Adapt: Adjust your expectations and let go of perfectionism. Flexibility reduces the strain of chronic stress.
4. Accept: Some stressors can’t be controlled—but they can be managed. Therapy can help process emotions and build resilience.

Simple daily practices—like exercise, mindfulness, regular sleep, and deep breathing — can reduce cortisol, improve energy, and naturally rebalance hormones over time.
If you notice ongoing fatigue, low libido, irritability, or persistent worry, it might be more than “just stress.” Consulting a psychologist or healthcare professional can help identify whether hormones and men emotional patterns are at play.
Therapy offers a space to understand stress triggers, restore balance, and develop coping skills that support both mental and hormonal health.
“Men’s mental health is not just about managing stress—it’s about reconnecting with yourself and learning that asking for help is an act of strength.”
— Dr. Arpita Biswas

Book a consultation with us at Scarborough Psychology Clinic—Compassionate Care for a Brighter Tomorrow.
Acevedo-Rodriguez, A., et al. (2018). Emerging Insights into Hypothalamic-Pituitary-Gonadal Axis Regulation and Interaction with Stress Signalling. Journal of Neuroendocrinology, 30(10), e12590. https://doi.org/10.1111/jne.
American Psychological Association. Stress effects on the body. https://www.apa.org/topics/
Cleveland Clinic. (2022). Testosterone: What It Is, Function & Levels. https://my.clevelandclinic.
Conway, A. (2021). The 4 A’s of Stress Relief. Mayo Clinic Health System. https://www.
Francis, K. T. (1981). The Relationship between High and Low Trait Psychological Stress, Serum Testosterone, and Serum Cortisol. Experientia, 37(12), 1296–1297. https://doi.org/10.1007/
Rojas-Zambrano, J. G., et al. (2025). Benefits of Testosterone Hormone in the Human Body: A Systematic Review. Cureus. https://doi.org/10.7759/
Walther, A., et al. (2018). Association of Testosterone Treatment with Alleviation of Depressive Symptoms in Men. JAMA Psychiatry, 76(1), 31–40. https://doi.org/10.1001/
Zitzmann, M. (2020). Testosterone, Mood, Behaviour and Quality of Life. Andrology, 8(6). https://doi.org/10.1111/andr.
Zueger, R., et al. (2023). Testosterone and Cortisol Responses to Acute and Prolonged Stress during Officer Training School. Stress Journal. Testosterone and cortisol responses to acute and prolonged stress during officer training school
I am a registered psychologist in private practice based in Toronto, Ontario, with over 30 years of clinical experience. I hold a Master’s degree, an M.Phil., and a Ph.D. in psychology. My extensive background spans various settings, including community agencies, hospitals, academic institutions, and private practice.
After eleven years of practice in India, I have dedicated the past two decades to providing diverse psychological services in Canada. I support clients in addressing a broad range of emotional and mental health concerns.